A Section that aims to investigate different aspects of the world of science, with particular attention to the most recent innovations
–
–
- Are the data on virus outbreaks and mortality real?
They are true in my opinion, but how can you even calculate rates when you have no clue about the real extent of the denominator (total no. of infected).
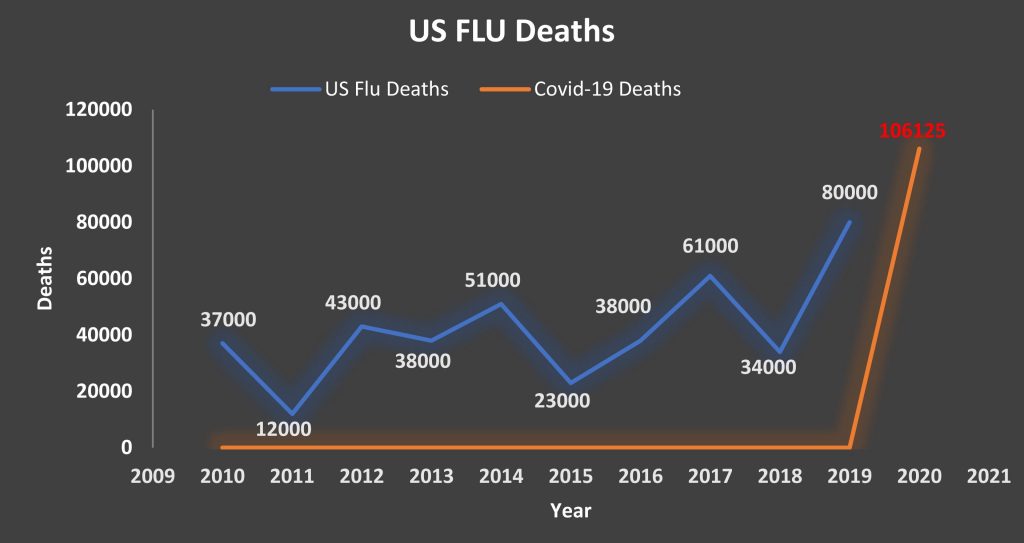
- According to some data, fewer people have died since the start of the pandemic than the total number that commonly die every year from complications due to the flu, Is that true?
People still forget this is in addition to, it is not replacing the flu. There is definitely a lot of overlap in the people who die from COVID-19 and those who would have died from the flu.
COVID-19 causes more severe disease than seasonal influenza. While many people globally have built up immunity to seasonal flu strains, COVID-19 is a new virus to which no one has immunity. That means more people are susceptible to infection, and some will suffer severe disease.
Many individuals who get coronavirus could maybe experience nothing worse than seasonal flu symptoms, but the overall profile of the disease, including its mortality rate, looks more serious. At the start of an outbreak the apparent mortality rate can be an overestimate if a lot of mild cases are being missed.
As cases of coronavirus infection proliferate around the world and governments have taken extraordinary measures to limit the spread, there is still a lot of confusion about what exactly the virus does to people’s bodies. The problem is that with this virus, you can have it, not have any symptoms, and still be infecting everyone around you before you feel sick. The Government knows this. That is why they shut the country down. On the international numbers, over 90% of cases will recover. But 9% will be seriously ill, and about 5% will require intensive care (ICU) and at least 2.5% will need ventilators.
- Is it true that this virus only kills immunosuppressed people? Why then did young people also die (albeit only a handful)? In short, what is the true nature and danger of this Virus?
SARS-CoV-2 is a pathogen which establishes intracellular latency. This elicits the NF-kB driven immune response. When this response becomes chronic and excessive, disease can result.
Chronic NF-kB activation is also seen in the diseases which predispose to severe COVID-19. Since the bar is already raised in these patients, the additional activation caused by COVID-19 can become extreme and life threatening. The NF-kB driven immune response attempts to prevent infection by downregulating the receptors used by pathogens to infect cells. This usually takes the form of decreased receptor expression on the cell membrane. The function of ACE-2 is to act as a counterbalance to the vasoconstrictive effects of angiotensin-2, by converting it to the vasodilator, angiotensin. Decreased expression of ACE-2 would therefore result in extreme vasoconstriction, resulting in hypertension, thrombosis, and an increase in ‘heart attacks’, as well as reduced uptake of oxygen from lungs. The virus enters via attachment to ACE2 receptors, which are expressed in certain cells found in the heart/kidneys/lungs etc…
Some research indicates that people with diabetes and hypertension are at greater risk due to treatment with ACE inhibitors, which inhibit a related ACE receptor. This increases the expression of ACE2, which helps their condition but may offer more points of entry and increase severity.
The mortality rates do seem to indicate the disease is worse in combination with these conditions, but I’m not sure how much research has been done to tie it directly to this factor.
The symptoms — fever, cough, shortness of breath — can signal any number of illnesses, from flu to strep to the common cold. Here is what medical experts and researchers have learned so far about the progression of the infection caused by this new coronavirus — and what they still don’t know.
- Are the security measures that are planned for the near future justified?
The lockdowns are supposed to buy time for the healthcare system to build up capacity and (hopefully) figure out a way to consistently reduce severity/duration of symptoms. Increased testing would also be more helpful than a vaccine, especially antibody testing as it would make it easier to gradually phase out lockdowns over the year. Flatten the curve means to slow down rate of transmission for ICU to cope but not stopping transmission altogether.
- What is our history with coronaviruses, and other flu like illness?
There are already 4 other Coronaviruses, this will be the 5th. The emerging consensus among epidemiologists is that the most likely outcome of this outbreak is a new seasonal disease — a fifth coronavirus. With the other four, people are not known to develop long-lasting immunity. If this one follows suit, and if the disease continues to be as severe as it is now, “cold and flu season” could become “cold and flu and COVID-19 season”.
Although little-known outside health care and virology circles, the current four “are already part of the winter-spring seasonal landscape of respiratory disease,” Adalja said. Two of them, OC43 and 229E, were discovered in the 1960s but had circulated in cows and bats, respectively, for centuries. The others, HKU1 and NL63, were discovered after the 2003-2004 SARS outbreak, also after circulating in animals. It is not known how long they’d existed in people before scientists noticed, but since they jumped from animals to people before the era of virology, it isn’t known whether that initial jump triggered widespread disease.
OC43 and 229E are more prevalent than other endemic human coronaviruses, especially in children and the elderly. Together, the four are responsible for an estimated one-quarter of all colds. “For the most part they cause common-cold-type symptoms”, said Richard Webby, an influenza expert at St. Jude Children’s Research Hospital. “Maybe that is the most likely end scenario if this thing becomes entrenched”.
- Can a useful Covid vaccine ever exist? Is there an optimal vaccine for a flu?
People love focusing on a vaccine, but realistically we are much more likely to have a viable treatment within the next 6-12 months. Vaccine is a good goal, but it’s not like one can happen anytime soon. What we really need is an effective way to treat symptoms, and that’s something that can be figured out a lot quicker than developing a new vaccine. There are diseases that have been with the species for thousands of years, and we have no vaccine for. They reinvent the Influenza vaccine every year. Additionally, vaccines for COVID-19 have built upon the already made but abandoned before final testing SARS vaccines. Novel virus vaccines are hard to make. I mean, vaccines are hard to make in general. The best candidate for SARS made it worse – since these diseases kill by triggering excess immune response it is a delicate balance. Stimulate the immune system enough to prevent the virus but not so much to make the disease lethal.
The 12-18 month time frame (could be more) for vaccine development is based on the assumption that a year of safety and efficacy testing is required. If the world cannot wait a year, we need to think outside the box and accelerate that. As long as it is safe, then it is better than no vaccine. However, the time frame is what it is because of the need to make sure it is safe. Realistically, it will be years until we have a vaccine for it, if one can even be developed, or if it is even worth doing. Right now, we have no real data on whether or not immunity lasts months, years…or if people are even immune at all.
The problem with creation of a broad spectrum antiviral is they’re usually modelled with mostly guess work from protein and DNA analysis and then in vitro samples need testing in live animals (usually pigs for anything meant to work on humans) and then you have to deal with vaccine toxicity and host resistance. So, the 18 months is going to be a ground-breaking time frame for a vaccine to SARS-NCov-2. It typically would take a decade for a vaccine to be produced for something like this. There is some possible good news coming out of antibody bioengineering, however.
Finally: At what stage of the disease (stage 1, 2, or 3? Please see the 3-stage mechanism of covid-19 below) was the treatment given to the patient that died? If it was given to the patient at stage 2 or 3, then it would most likely not help, and the patient would certainly die. There are different repurposed treatments being tested right now for each stage of the virus so we can collect more data. Do we have any data on the number of people that died from taking hydroxychloroquine while being treated for covid-19? Was it the hydroxychloroquine or the virus that killed them? Is it possible that this medication did not work because they were already at stage 2 or 3 of the disease? We need to collect more scientific data.
I think that we should investigate viral infection/symptoms more over the late stage development of ARDS. If we can stop the onset of pneumonia by detecting the early signs of covid-19, then doctors can prescribed these repurposed covid meds that have been proven to save some people’s lives right away (although they are not 100% effective, just need to make sure they don’t have deadly side effects) and patients can take them immediately to prevent themselves from getting pneumonia.
If there is a way to stop COVID-19, it will be by blocking its proteins from hijacking, suppressing, and evading humans’ cellular machinery.
–
STAGE I: STOP THE VIRUS FROM GETTING INTO A CELL
One possible mechanism for the much-hyped HYDROXYCHLOROQUINE, the malaria drug Trump is fixated on, may be inhibiting this spike-activation process.
STAGE II: STOP THE VIRUS FROM REPLICATING
Replication is a relatively complicated step, which makes it a ripe target for antivirals. “There’s many, many proteins involved … there’s many potential targets,” says Melanie Ott, a virologist at the Gladstone Institutes and UCSF. For example, REMDESIVIR, an experimental antiviral that is in clinical trials for COVID-19, targets the viral protein that copies the RNA, so the genome-copying step goes awry.
Rather than directly fighting the virus, ACTEMRA is an anti-inflammatory drug that may help alleviate symptoms in COVID-19 patients. In particular, some severe cases have been marked by an overactive immune response that can damage the lungs. This testing will help answer if Actemra can help these patients.
STAGE III: STOP THE IMMUNE SYSTEM FROM GOING HAYWIRE
Another way to treat COVID-19, then, is by treating the immune response, rather than the virus itself. Drugs for quelling the immune system in these patients are now being repurposed in clinical trials for COVID-19. Randy Cron, a rheumatologist at the University of Alabama, is planning a small trial for ANAKINRA, an immunosuppressant currently approved to treat rheumatoid arthritis. Other trials are repurposing yet other drugs on the market, such as TOCILIZUMAB and RUXOLITINIB , which were originally developed for arthritis and diseases of the bone marrow, respectively. Treating a viral infection by damping down the immune system is especially tricky to balance, because the patient still needs to clear the virus.
Please stay safe and healthy.
Hossam Ibrahim








Amazing, detailed article
awesome. great article !
grazie Uki . questo blog e’ sempre piu’ interessante
Great insight . A better scientific understanding.
Maravilhoso o artigo! A linguagem acessível para quem não é da área cientifica, super informativo a e embasado em estudos sérios.
Well done man
Very well detailed information
spettacolare!
dovreste proporlo alla task force dei virologi che da noi non ci hanno capito un caxxo
very interesting insights.
now I know much more.
it must be said that what the doctors have told us so far was not always correct